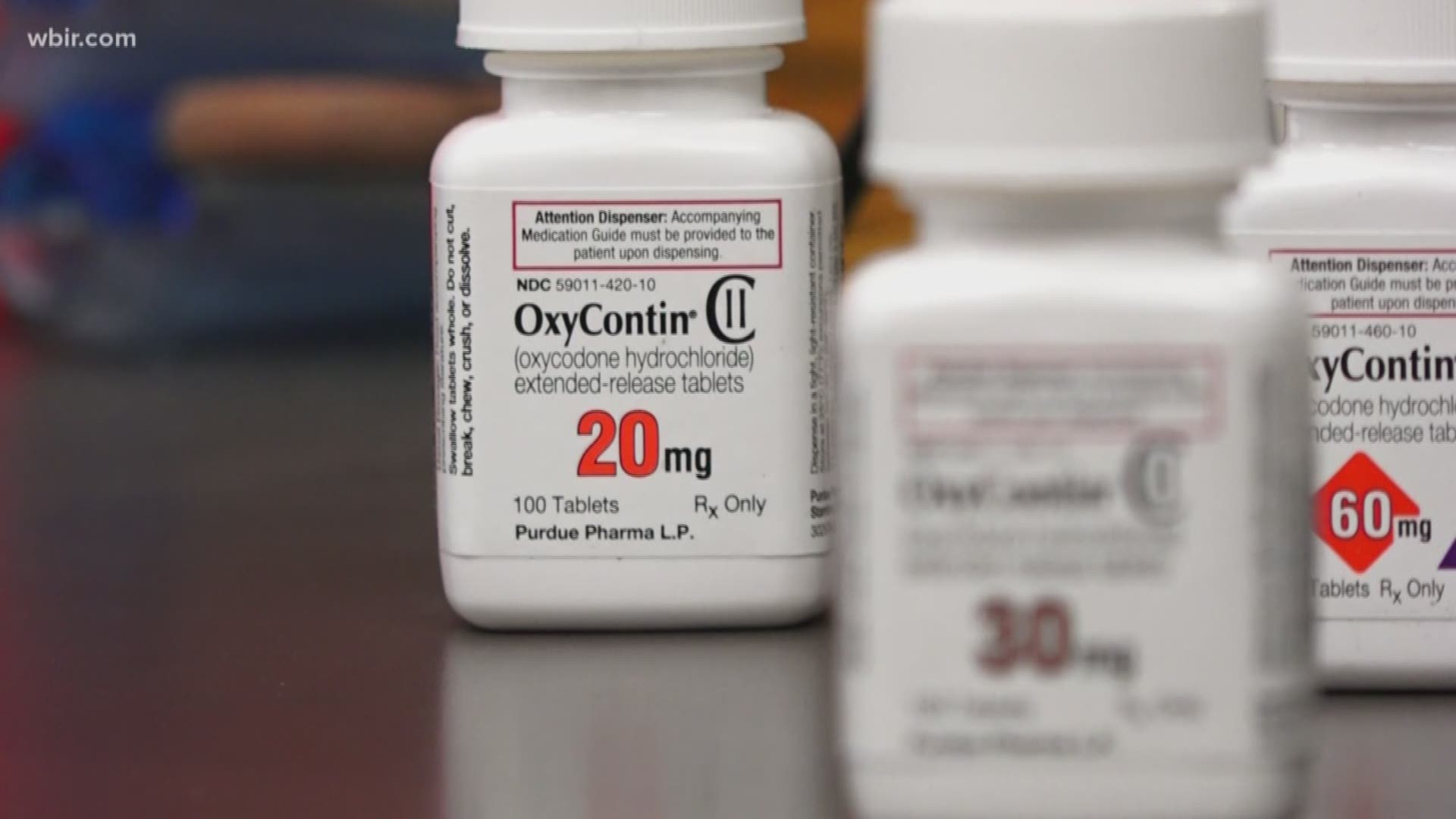
One of the best known pain medications will soon be out of network for 3.4 million BlueCross customers in Tennessee.
The company announced Thursday it will no longer cover OxyContin prescriptions beginning in 2019. Instead, it will pay for two other opioid prescriptions the it says are less likely to be abused.
"Patients have found ways around the abuse deterrent mechanisms that are in OxyContin which allows them to still abuse them unfortunately," Josh Gass, a Knoxville pharmacist, said.
Because of that, BlueCross is following providers like Cigna and Tenncare who already no longer pay for the drug.
"If you're a patient who has received OxyContin in the past, this change in BlueCross BlueShield's formulary doesn't keep you from getting the product or from a doctor prescribing it for you. They are just saying they will no longer cover it," Gass said.
The State of Tennessee is currently suing the maker of OxyContin. It says Perdue Pharma pushed doctors to prescribe medication that some say served as a gateway to the opioid crisis.
Stephanie Vanterpool, the medical director for UT Medical Center's pain management clinic, says the BlueCross change today is for the better.
"It's a positive direction in terms of turning attention away from medications that could be possibly manipulated."
But she says doctors need to change the way they approach pain in general and move away from opioid medications.
"Pain often has multiple causes, and while oxycodone which is one of the opioid medications treats the pain, it doesn't actually cover up the source. We use a phrase here treat the source not the score, that means treat the source of the pain not just the pain score."
BlueCross is also lowering the strength threshold of opioids it will cover and limiting first-time, short-term prescriptions to seven days.